In-Depth Overview of Laparoscopic Salpingo-Oophorectomy Procedure Steps: A Modern Approach in Gynecological Surgery
In the realm of advanced gynecological surgeries, the laparoscopic salpingo-oophorectomy stands out as a minimally invasive, highly effective procedure performed by specialized obstetricians and gynecologists like those at DrSeckin.com. This procedure involves the removal of one or both fallopian tubes and ovaries through small incisions with the aid of a laparoscope, leading to faster recovery times and fewer complications compared to traditional open surgeries.
Understanding the Significance of Laparoscopic Salpingo-Oophorectomy
The laparoscopic salpingo-oophorectomy is frequently performed for a range of medical reasons, including ovarian cysts, ovarian cancer, endometriosis, tubal ligation, or prophylactic removal in high-risk patients with genetic predispositions such as BRCA mutations. Its benefits include minimal scarring, reduced postoperative pain, shortened hospital stay, and quicker return to daily activities.
Essential Preparations Before the Procedure
Effective preparation is key to ensuring safety and success in laparoscopic salpingo-oophorectomy procedures. Patients are typically advised to undergo preoperative evaluations, including blood tests, imaging studies, and anesthetic assessments. It’s crucial to discuss any medications or allergies with the surgical team. Fasting guidelines are strictly followed to prevent complications during anesthesia.
Step-by-Step Breakdown of the Laparoscopic Salpingo-Oophorectomy Procedure Steps
1. Anesthesia Administration and Patient Positioning
Under general anesthesia, the patient is carefully positioned in a dorsal lithotomy position with arms secured. Positioning ensures optimal surgical access and minimizes risks of nerve injury. The operating table is adjusted to facilitate a clear view of the pelvis.
2. Creation of Pneumoperitoneum
An initial small incision is made, typically at the umbilical region, to insert a Veress needle or perform an open (Hasson) technique for access. Carbon dioxide gas is insufflated into the abdominal cavity, creating a pneumoperitoneum that provides working space for the laparoscope and instruments.
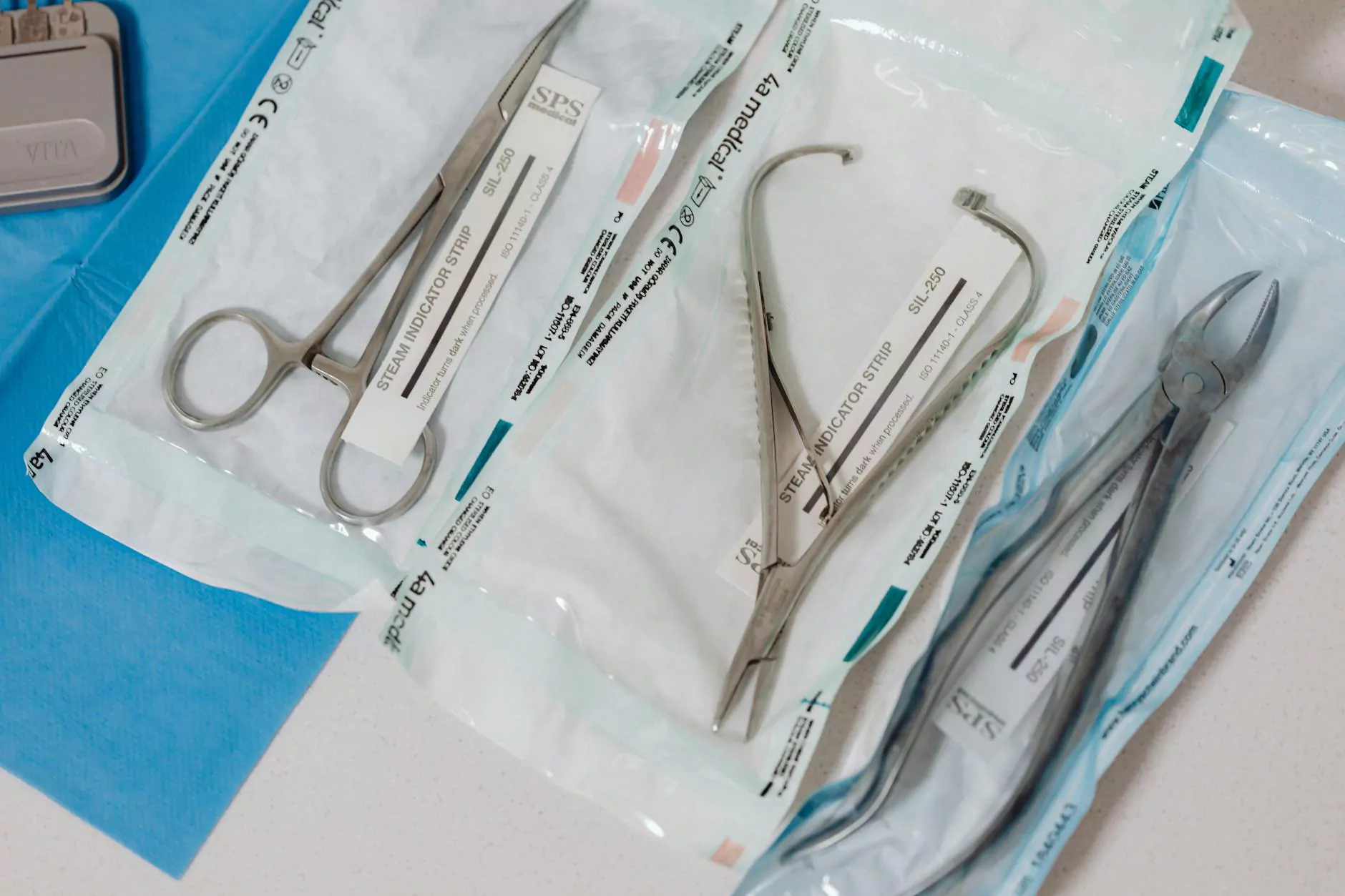
3. Insertion of the Laparoscope and Surgical Ports
The laparoscope—a slender camera-equipped instrument—is introduced through the umbilical port. Additional small incisions are made in the lower abdomen to insert trocars, which serve as channels for surgical tools. Precise placement is vital to prevent injury to surrounding tissues.
4. Systematic Exploration of the Pelvic Cavity
Experienced surgeons meticulously examine the pelvis, identifying the ovaries, fallopian tubes, uterus, and neighboring structures. Any pathological findings, such as cysts or adhesions, are documented. This thorough exploration guides the removal process and enhances surgical safety.
5. Dissection and Isolation of Target Structures
The next step involves carefully dissecting the ovarian and tubal ligaments. Ligatures or energy devices like bipolar cautery and ultrasonic scalpels are employed to control blood vessels and minimize bleeding. The surgeon isolates the ovary and fallopian tube from surrounding tissues, ensuring clear separation.
6. Detachment and Removal of the Ovarian and Fallopian Structures
Using precise energy application, the surgeon completely detaches the ovary and fallopian tube from their vascular and ligamentous attachments. The specimen is carefully grasped and placed into an endoscopic retrieval bag to prevent spillage or dissemination of tissue.
7. Specimen Extraction
The reproductive structures are extracted through the enlarged umbilical port or another strategically chosen site. In some cases, the specimen may be morcellated (cut into smaller pieces) within the retrieval bag to facilitate removal, especially if the ovary or tube is large.
8. Hemostasis, Inspection, and Closure
After removal, meticulous inspection ensures complete hemostasis, preventing postoperative bleeding. The surgical field is irrigated, and any residual adhesions or bleeding points are addressed. Once confirmed that no complications exist, the laparoscopic ports are closed with sutures or skin staples.
Key Advantages of the Laparoscopic Salpingo-Oophorectomy Technique
- Minimally invasive approach: Smaller incisions lead to less pain and scarring.
- Reduced recovery time: Patients often return to normal activities within days.
- Enhanced safety: Precise visualization reduces intraoperative complications.
- Lower risk of infections and complications: Decreased postoperative morbidity.
- Cosmetically favorable: Minimal scarring and better aesthetic outcomes.
Postoperative Care and Expected Outcomes
Following laparoscopic salpingo-oophorectomy, patients are closely monitored for signs of bleeding or infection. Analgesics are provided to manage discomfort, and activity is gradually resumed. Most patients experience minimal pain, and hospital stays are typically short, often less than 24 hours for uncomplicated cases.
Risks and Considerations
As with any surgical procedure, potential risks include bleeding, infection, damage to surrounding organs, and anesthesia-related complications. However, the advanced skills of specialists at DrSeckin.com significantly mitigate these risks, ensuring safe and effective outcomes.
Choosing the Right Specialist and Facility
Highly trained obstetricians and gynecologists with extensive experience in minimally invasive surgery are crucial for optimal results. Facilities equipped with state-of-the-art laparoscopic equipment, comprehensive preoperative and postoperative care, and a multidisciplinary approach further enhance the success rate of these procedures.
Conclusion: Embracing the Future of Gynecological Surgery
The laparoscopic salpingo-oophorectomy procedure steps exemplify the remarkable advancements in modern gynecological surgery. It embodies safety, precision, and patient-centered care. If you are considering or require this procedure, consulting with highly qualified specialists like those at DrSeckin.com ensures that you receive the best treatment tailored to your individual health needs.
By understanding the meticulous and systematic nature of the laparoscopic salpingo-oophorectomy process, patients and providers can work together towards achieving optimal outcomes with minimal discomfort and swift recovery. Embracing minimally invasive techniques paves the way for a healthier, more comfortable experience in gynecological healthcare.
laparoscopic salpingo oophorectomy procedure steps