Deep Vein Thrombosis (DVT): A Complete Guide to Prevention, Diagnosis, and Treatment

Deep vein thrombosis (DVT) is a potentially serious condition characterized by the formation of a blood clot in the deep veins, typically in the legs. As a leading component of vascular medicine, understanding deep vein thrombosis is essential for both medical professionals and the general public interested in vascular health. This article provides a comprehensive examination of DVT—covering its causes, risk factors, symptoms, diagnostic procedures, innovative treatments, and how specialized care can dramatically improve patient outcomes.
Understanding Deep Vein Thrombosis: Definition and Importance
Deep vein thrombosis occurs when a blood clot, also known as a thrombus, develops in the deep venous system, which is responsible for returning deoxygenated blood from the lower limbs and pelvis back to the heart. Due to the potential risk of the clot dislodging and causing a pulmonary embolism, DVT is recognized as a critical component of venous thromboembolic disease (VTE).
Effective management and early intervention in deep vein thrombosis are crucial because untreated cases can lead to complications such as post-thrombotic syndrome, chronic venous insufficiency, and even fatal pulmonary embolisms. With the advancements in vascular medicine, particularly in diagnostics and minimally invasive treatments, patients today have access to more effective, personalized care plans.
Causes and Risk Factors of Deep Vein Thrombosis
Primary Causes of DVT
- Venous Stasis: Occurs when blood flow slows down or becomes stagnant, often due to immobility or prolonged bed rest.
- Endothelial Injury: Damage to the blood vessel lining caused by trauma, surgery, or inflammation which predisposes to clot formation.
- Hypercoagulability: Abnormal blood clotting tendencies often linked to genetic traits, certain medications, pregnancy, or malignancies.
Key Risk Factors
- Prolonged Immobility: Long airplane or car journeys, hospital stays, or paralysis increase DVT risk.
- Age: The likelihood of developing DVT rises significantly after age 40.
- Obesity: Excess weight puts additional pressure on veins, impeding blood flow.
- Pregnancy and Postpartum Period: Hormonal changes and increased abdominal pressure contribute to risk.
- Genetic Predispositions: Conditions like factor V Leiden mutation or prothrombin gene mutation.
- Cancer and Its Treatments: Malignancies and chemotherapy elevate thrombotic risk.
- Use of Hormonal Contraceptives or Hormone Therapy: Estrogen-based treatments can increase clot formation.
Recognizing the Symptoms of Deep Vein Thrombosis
While some cases of deep vein thrombosis are asymptomatic, common signs and symptoms include:
- Swelling: Notably in one leg or arm, often persistent or worsening.
- Pain or Tenderness: Usually in the calf or thigh, often described as aching or cramping.
- Skin Changes: Redness, warmth, or discoloration over the affected area.
- Enlargement of the Vein: Visible superficial veins or cord-like structures.
- Difficulty Walking: Due to discomfort or swelling.
If you experience symptoms suggestive of deep vein thrombosis, prompt medical consultation is essential to prevent severe complications.
Diagnosing Deep Vein Thrombosis: Modern Techniques and Best Practices
Initial Clinical Evaluation
Medical professionals utilize thorough patient histories and physical examinations focusing on signs indicative of DVT. However, due to symptom overlap with other conditions, definitive diagnostic procedures are critical.
Advanced Diagnostic Modalities
- D-dimer Test: A blood test measuring fibrin degradation products, elevated levels suggest active clot formation but are not specific to DVT.
- Duplex Ultrasound: The first-line imaging technique combining B-mode imaging and Doppler flow studies to visualize clot presence and blood flow.
- Ventilation-Perfusion Scanning (V/Q Scan): Used mainly when ultrasound results are inconclusive, especially in cases involving pelvic DVT.
- Venography: An invasive but highly precise imaging method involving contrast dye, reserved for complex cases.
Utilizing these diagnostics allows for accurate identification of deep vein thrombosis, enabling tailored treatment protocols.
Innovative and Effective Treatments for Deep Vein Thrombosis
Anticoagulant Therapy: The Cornerstone of DVT Management
Anticoagulants, such as heparin, warfarin, and direct oral anticoagulants (DOACs) like rivaroxaban and apixaban, are primary treatments. They inhibit clot formation, prevent growth, and reduce embolic risks.
Thrombolytic Therapy
In severe cases, specifically extensive DVT or iliofemoral thrombosis, thrombolytic agents like tissue plasminogen activator (tPA) may be administered to dissolve clots, often via catheter-directed approaches in specialized vascular centers.
Minimally Invasive Interventions
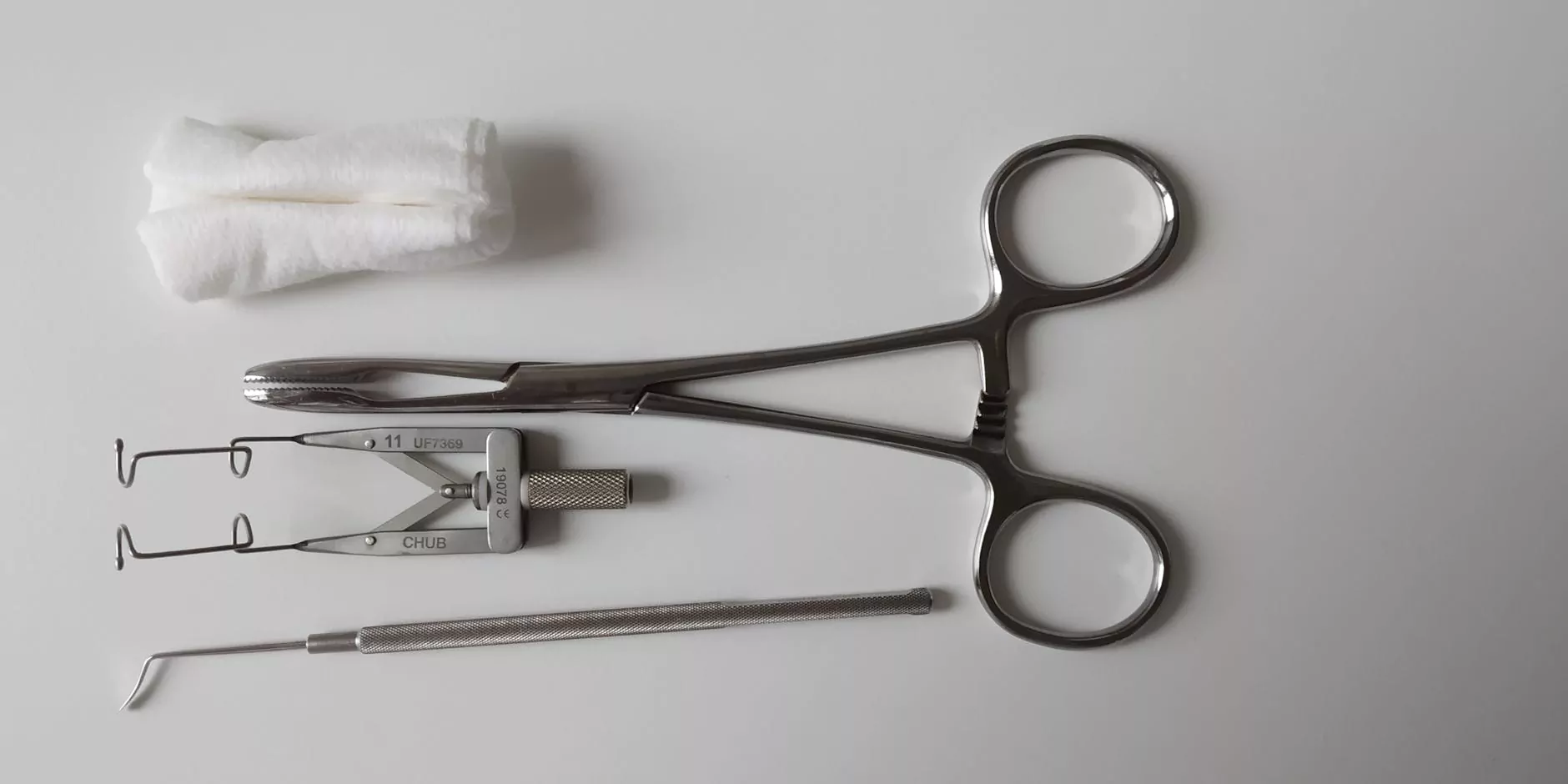
- Catheter-Directed Thrombectomy: Mechanical removal of clots using specialized devices, significantly reducing clot burden with minimal recovery time.
- Laser or Ultrasound-Assisted Thrombolysis: Enhances the effectiveness of clot dissolution.
- Inferior Vena Cava (IVC) Filters: Devices inserted temporarily or permanently to prevent large clots from reaching the lungs in high-risk patients.
Long-Term Management and Prevention
After initial treatment, strategies include compression therapy (graduated compression stockings), lifestyle modifications, and ongoing anticoagulation to diminish recurrence risk. Addressing underlying risk factors, such as weight management and smoking cessation, is also essential.
Advanced Vascular Medicine Settings: Why Choose Experts for DVT Care
Leading vascular medicine practices, like those at trufflesveinspecialists.com, offer cutting-edge diagnostics, personalized treatment plans, and minimally invasive procedures. Their multidisciplinary approach ensures comprehensive patient care, from prevention to post-treatment management.
Specialized centers also incorporate novel therapies and participate in ongoing clinical trials, contributing to the evolution of DVT treatment protocols. This ensures that patients benefit from the latest innovations in vascular medicine and reduce the risk of complications.
The Future of Deep Vein Thrombosis Treatment and Prevention
The landscape of DVT management continues to evolve with breakthroughs in biomedical research, nanotechnology, and personalized medicine. Emerging therapies focus on targeted drug delivery systems, gene therapies, and bioengineering solutions that promise higher efficacy, fewer side effects, and better quality of life for patients.
Preventive strategies are also gaining prominence, emphasizing risk stratification, early screening, and patient education to reduce incidence rates globally.
Conclusion: Prioritizing Vascular Health to Combat DVT
Understanding deep vein thrombosis at a systemic level empowers both healthcare providers and patients to recognize symptoms early, pursue precise diagnostics, and implement effective treatment strategies. As vascular medicine advances, the outlook for individuals affected by DVT continues to improve dramatically. Accessing specialized care from reputable centers like Truffle Vein Specialists ensures that patients receive the highest quality of care designed to prevent life-threatening complications and promote optimal vascular health.
Stay informed, stay proactive, and prioritize your circulatory health to overcome the challenges posed by deep vein thrombosis.